By CRISTINA JANNEY
Hays Post
Is that runny nose and cough COVID or just your run-of-the-mill seasonal allergies?
Doctors at the University of Kansas Health System tried to give viewers tips on how to distinguish between the two during their daily news briefing Wednesday.
Dr. Steve Stites, chief medical officer, and Dr. Dana Hawkinson, medical director of infection prevention and control, were joined by Dr. Selina Gierer, specialist in allergy, immunology and rheumatology medicine, and ear, nose and throat surgeon Dr. Keith Sale.
Gierer said Kansas has reached its peak allergy season. Children are also returning to school and can be exposed to viral infections.
"It is always a challenge when we go back to school when kids get any viral infection on top of season allergies trying to pick a part what's an illness and what is an allergy symptom," she said.
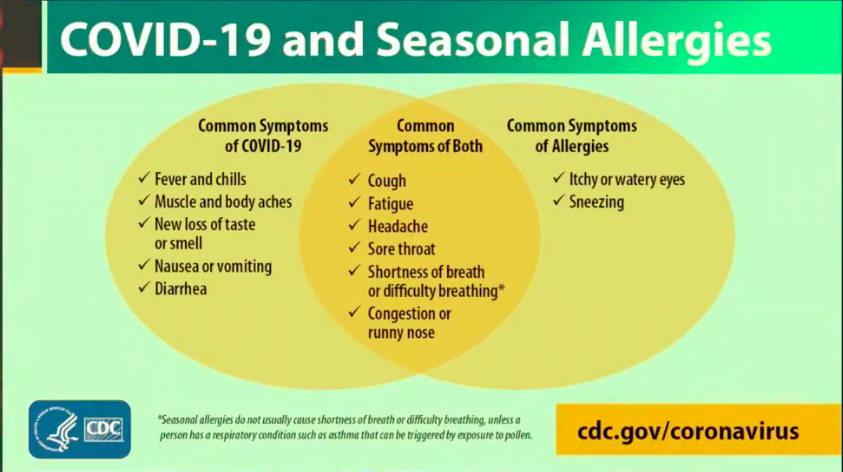
Itchy and water eyes as well as sneezing are common symptoms of allergies, but not of COVID-19.
Then there is an overlap zone for both allergies and COVID, Gierer said.
These include cough, fatigue, headache, sore throat, shortness of breath and runny nose.
"Ultimately, if you are having fever, if your symptoms are not typical for your allergy symptoms," Gierer said, "perhaps this is not a typical allergy season for you.
"If you are having cough, if you are having congestion and you are having change in your sense of smell, it's time for you to be thinking about contacting your doctor to get tested for coronavirus."
She suggested keeping control of your allergy symptoms and avoiding people who are sick.
Monitor your triggers, such as dust, mold, pollen or animals. Monitor the local pollen count. Stay on your allergy medications.
"If you know you are going to be doing yard work, and the next day you feel itchy and drippy and sneezy, you can probably attribute that to your allergies and not an acute onset of coronavirus," Gierer said.
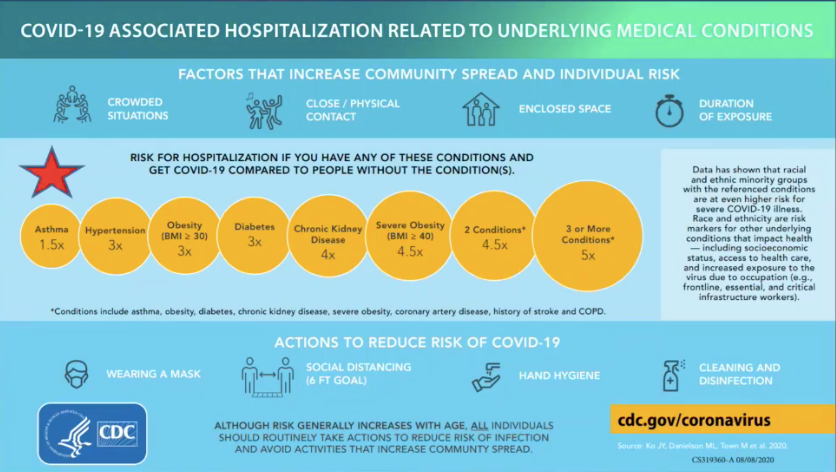
Asthma is an underlying medical condition that increases the likelihood of complications from coronavirus. However, it is on the lower end of the range of complicating factors.
Asthma is much less common to cause complications than obesity and hypertension, Gierer said.
However, one of the biggest triggers of asthma is a viral infection. She said it is also important to keep your asthma under control by staying on medications, avoiding triggers and keeping a 30-day supply of medication on hand.

Dr. Sale saw a patient in his clinic who was having typical symptoms for allergies, such as a runny nose, but was not getting better on her normal medications.
She thought she had a sinus infection or something else. A friend from out of town had visited the week before. She was tested for COVID and was surprised with a positive COVID test, Sale said.
Sale said his office is taking COVID precautions, including using PPE, hand sanitizing between patients and patients wearing masks unless their nose or mouth is being examined.
Gierer said allergy medication or a rescue inhaler will probably not help with COVID-19 symptoms.
Sale said fatigue may be common to both allergies and COVID, but the persistence of the symptom may be a sign of the later.
Gierer said, "If the allergy medications are not working, that might trigger you to think there is something else going on."
Hawkinson said scientists are working to combine testing for flu and COVID-19. He said if a patient has a nasal swab for COVID-19, a lab could use that same sample to test for flu and RSV.
RSV, is a common respiratory virus that usually causes mild, cold-like symptoms. Most people recover in a week or two, but RSV can be serious, especially for infants and older adults, according the Centers for Disease Control.
The flu season is in full swing in South Africa and Australia and has been lighter this year there than in years past, Hawkinson said. He said that could be in part to mask use and increased hand washing.
KU Med is working on mass flu vaccination at this time.
Gierer urged members of the public to get flu vaccines. That is usually recommended starting in October.
The doctors also gave tips on staying in good general health.
You can naturally boost your immune system by getting adequate sleep, eating a healthy diet, as well as hand washing and staying away from people who are sick.
Those tips can help with COVID-19, flu or RSV.
Sale also said caring for your mental health can have an effect on maintaining physical health, which includes socializing in a safe way.






